Decades of research have identified the major risk factors for head and neck cancers (HNC). Tobacco and alcohol habits account for a significant portion of the global incidence of this disease. In recent years, oral infection with the human papillomavirus (HPV) has been identified as a risk factor mainly for oropharyngeal cancers (a subgroup of HNC).
However, several important questions remain unanswered: i) does tobacco smoking at all ages entail the same risk of developing HNC? ii) does smoking after oral HPV infection influence an individual’s risk? iii) how long is the latency of tobacco smoking in HNC? These questions concern the timing of exposure and the time from exposure to disease.
The life course approach in epidemiology can provide a framework to answer the above questions.
The overall objective of this Ph.D. project is to compare life course models of behavioral risk factors for HNC in two countries with different socio-cultural circumstances and economic development.
We used data from the HeNCe Life study, a hospital-based case-control study conducted in Canada and India using similar protocols. Cases were newly diagnosed subjects with primary squamous cell carcinomas of the mouth, pharynx, and larynx at stages I-IV recruited from various hospitals. Control subjects were non-cancer patients selected from several outpatient clinics in a hospital located in the same catchment area as the cases and frequency-matched to cases according to age and sex. Life course information on a wide range of risk factors was collected using structured questionnaires with the help of a life grid.
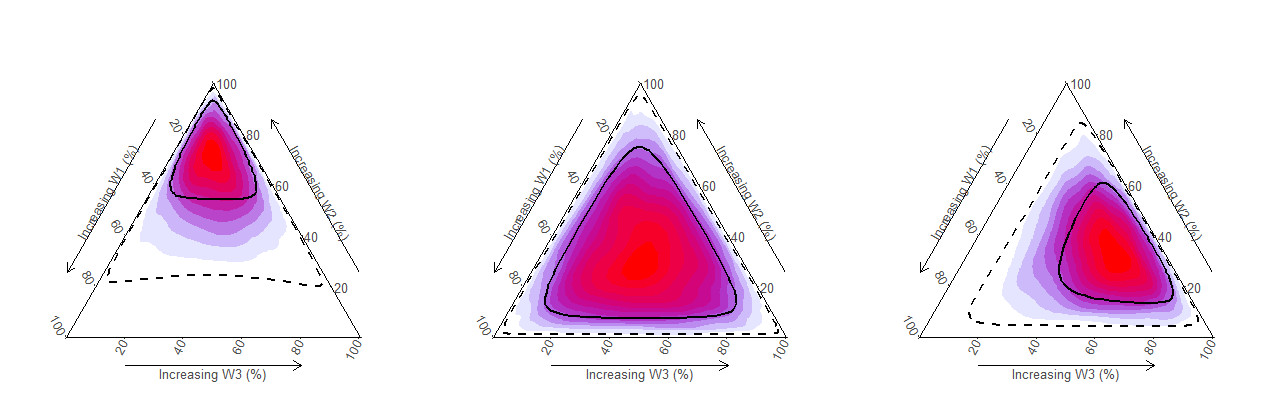
We estimated and compared the average life course trajectories of smoking and betel quid chewing habits among HNC cases and controls in two countries. Motivated by the complexity of data, we developed the Bayesian relevant life course exposure model (BRLM) to investigate life course hypotheses of continuous exposure. Using the BRLM, we investigated which life course hypothesis best describes the association between tobacco smoking and HPV-negative oral cancers in two countries. We also estimated the latency function for tobacco smoking with regards to risk of HNC among HPV- positive and negative participants.
Average life course trajectories of smoked tobacco habits in two countries showed similar patterns with a hump shape. Compared to the controls, HNC cases had a higher intensity of smoking during most of their life course in both countries. BRLM identified the ‘true’ life course hypothesis in all combinations of hypotheses and sample sizes tested in the simulation study. For betel quid chewing <= 20 years of age was identified as a sensitive period associated with increased risk of developing oral cancer later in life.
Results from Manuscript III are suggestive of a later life sensitive period for tobacco smoking in relation to risk of HPV-negative HNC in both Canada and India.
Finally, results from Manuscript IV suggest a temporal interaction between HPV infection and tobacco smoking in relation to risk of HNC in Canada.
Life course trajectories of behavioral risk factors are culturally different, signifying the need for a life course approach in risk assessment studies in cancer. BRLM can provide easily interpretable estimates for probabilities of life course hypotheses. There are periods in life which are more sensitive to insults from behavioral risk factors leading to risk of HNC in later life. Replication studies across different geographical regions and using birth cohort data are essential next steps.